Table of Contents
Opportunities for healthcare professionals and students to contribute their skills and knowledge in underserved communities are often structured as organized initiatives. These initiatives facilitate the delivery of medical assistance, health education, and capacity building in areas with limited access to healthcare services. A doctor spending a week providing care in a rural clinic exemplifies participation in such an organized initiative.
Participation in these structured opportunities yields significant benefits, fostering professional development, expanding cultural understanding, and contributing to improved health outcomes for vulnerable populations. Historically, such initiatives have played a critical role in addressing health disparities and responding to global health crises, showcasing the dedication of medical personnel to humanitarian efforts worldwide.
The following sections will delve into various aspects of these initiatives, including the types of programs available, the locations they serve, the requirements for participation, and the overall impact they have on both the volunteers and the communities they assist.
Navigating Medical Volunteer Programs
Engaging in structured opportunities for healthcare professionals requires careful planning and consideration. The following tips offer guidance to ensure a productive and ethical experience.
Tip 1: Align Skills with Program Needs. Thoroughly assess one’s medical expertise and match it with the specific requirements of the structured opportunity. A surgeon, for example, should seek opportunities where surgical skills are directly applicable.
Tip 2: Research Program Credibility. Prioritize reputable organizations with a proven track record of ethical and effective service delivery. Investigate the organization’s history, affiliations, and impact metrics.
Tip 3: Understand Cultural Sensitivity. Prepare for cultural differences by researching the customs, beliefs, and communication styles of the host community. Participate in pre-departure training on cultural awareness.
Tip 4: Secure Proper Licensing and Insurance. Verify that medical licenses are valid and transferable to the program’s location. Obtain comprehensive medical malpractice and travel insurance coverage.
Tip 5: Develop Realistic Expectations. Recognize that resources may be limited, and the scope of practice may differ from familiar settings. Embrace adaptability and resourcefulness.
Tip 6: Prioritize Patient Safety and Confidentiality. Adhere to strict ethical guidelines and maintain patient confidentiality at all times. Respect local medical protocols and seek guidance when necessary.
Tip 7: Document Experiences and Share Knowledge. Keep a detailed record of activities, challenges, and lessons learned. Contribute to the program’s knowledge base by sharing insights and best practices.
By adhering to these guidelines, individuals can maximize the positive impact of their participation in structured opportunities, while safeguarding their well-being and upholding professional standards.
The subsequent sections will address the long-term effects of these experiences on both the individual volunteers and the communities they serve, providing a comprehensive understanding of the overall benefits.
1. Ethical Considerations
Ethical considerations form the bedrock of responsible engagement in organized medical service. The potential for exploitation of vulnerable populations necessitates rigorous adherence to ethical principles. Unregulated interventions, however well-intentioned, can inflict unintended harm, undermining local healthcare systems and fostering dependency. For example, providing free medical services without addressing underlying social determinants of health, such as sanitation and access to clean water, may offer only temporary relief while failing to empower the community for long-term well-being. Conversely, a sustainable initiative would collaborate with local healthcare providers to build capacity and address systemic issues.
Adherence to established ethical frameworks, such as those outlined by the World Medical Association and various national medical boards, is paramount. Transparency in program objectives, resource allocation, and data collection practices is crucial to building trust and accountability. Informed consent, cultural sensitivity, and respect for patient autonomy must be integral components of every interaction. Consider the example of a program that fails to adequately obtain informed consent from patients before conducting medical research; this constitutes a clear violation of ethical principles and can have devastating consequences for the individuals involved. Similarly, imposing medical practices that conflict with local cultural beliefs can erode trust and hinder the program’s effectiveness.
In summary, ethical considerations are not merely peripheral concerns, but rather fundamental prerequisites for engaging in structured medical service. Prioritizing ethical conduct safeguards the well-being of vulnerable populations, fosters sustainable development, and upholds the integrity of the medical profession. Overlooking these principles can result in unintended harm and erode the very foundations of trust upon which effective healthcare delivery depends. Future discussions should address specific ethical dilemmas that often arise and offer practical strategies for navigating these complex situations.
2. Skill Application
The effective deployment of expertise is central to the success and ethical soundness of structured medical service. The alignment of professional capabilities with the specific needs of a community dictates the impact of the volunteer effort. Mismatched skills can lead to ineffective interventions or, worse, cause harm.
- Diagnosis and Treatment Proficiency
Proficient diagnostic and therapeutic skills are essential. A program delivering primary care requires clinicians capable of accurately diagnosing common ailments and prescribing appropriate treatments within available resources. For instance, a physician volunteering in a remote clinic may need expertise in managing infectious diseases and providing prenatal care with limited diagnostic tools.
- Surgical Specialization
Surgical roles demand specific qualifications and experience. Programs conducting surgical interventions necessitate skilled surgeons with expertise relevant to the procedures being performed. An orthopedic surgeon should only participate in programs where their skills in fracture repair and joint replacement are directly applicable. Insufficient expertise could lead to complications and harm patients.
- Public Health Expertise
Public health professionals contribute through preventative strategies and community education. Their skills are vital for addressing underlying health determinants and promoting healthy behaviors. For example, a public health nurse might implement a program to improve sanitation practices or conduct educational workshops on disease prevention, focusing on interventions that will create lasting change.
- Training and Mentorship
Transferring skills to local healthcare providers enhances long-term sustainability. Seasoned professionals can train local medical personnel in essential skills, empowering them to provide ongoing care after the program’s conclusion. A senior physician mentoring junior doctors in a rural hospital is a prime example of how skill transfer can create a lasting legacy.
The successful application of specialized skills within structured opportunities necessitates careful assessment, planning, and ongoing evaluation. Matching individual abilities to program requirements maximizes positive impact, promoting effective and ethical healthcare delivery. The ultimate goal is to empower local communities to sustain their own health improvements.
3. Cultural Sensitivity
Within organized medical service, cultural sensitivity represents a core competency, influencing the efficacy and ethical dimensions of healthcare interventions. Failure to recognize and respect cultural nuances can impede communication, undermine trust, and compromise health outcomes.
- Communication Styles
Variations in communication styles significantly impact patient interactions. Direct communication, common in some cultures, may be perceived as disrespectful in others, where indirect approaches are preferred. Medical personnel must adapt their communication to align with the cultural norms of the community served. For instance, avoidance of direct eye contact might signify respect in certain cultures, while in others, it could be interpreted as evasiveness or dishonesty. Volunteers need to be observant and receptive to these subtleties to build rapport and elicit accurate patient information.
- Beliefs About Health and Illness
Cultural beliefs profoundly shape perceptions of health, illness, and treatment. Biomedical models of disease may clash with traditional healing practices. Understanding and respecting these beliefs is essential for effective collaboration and patient adherence. For example, a community might attribute illness to spiritual causes rather than biological pathogens. Disregarding these beliefs can lead to resistance to conventional medical interventions. A culturally sensitive approach involves integrating traditional practices where appropriate and explaining biomedical concepts in a culturally relevant manner.
- Decision-Making Processes
Decision-making processes related to healthcare often vary across cultures. In some societies, individual autonomy is paramount, while in others, family or community elders hold significant influence. Medical volunteers must navigate these dynamics with sensitivity, ensuring that all relevant parties are involved in the decision-making process. For example, in some cultures, a male relative may need to provide consent for a female patient’s treatment. Respecting these cultural norms is crucial for building trust and ensuring that patients receive appropriate care.
- Dietary Practices and Food Restrictions
Dietary practices and food restrictions are integral aspects of culture that influence health outcomes. Medical interventions that disregard these practices can be ineffective or even harmful. Volunteers must be aware of common dietary restrictions and adapt treatment plans accordingly. For instance, certain religious or cultural groups may adhere to strict dietary laws that prohibit the consumption of specific foods. Providing culturally appropriate meals and nutritional guidance is essential for promoting patient well-being and fostering trust.
The integration of cultural sensitivity into medical service enhances the potential for positive outcomes, fostering collaborative relationships and promoting equitable healthcare delivery. A comprehensive understanding of these multifaceted cultural dimensions enables healthcare providers to tailor their interventions to the specific needs of the communities they serve, resulting in improved health outcomes and increased community trust in medical interventions.
4. Sustainability Impact
The concept of sustainability extends beyond environmental concerns to encompass the enduring positive effects of interventions within communities served by medical volunteer initiatives. Long-term benefits, rather than short-term aid, define a program’s true success and ethical standing. The following facets illustrate the critical components of sustainable impact in this context.
- Capacity Building
Empowering local healthcare providers through training and mentorship is paramount for lasting change. Instead of merely delivering services, initiatives should transfer knowledge and skills, enabling communities to manage their own healthcare needs independently. A volunteer program that trains local nurses in advanced wound care techniques, for example, creates a self-sufficient resource that remains long after the volunteers depart. Failure to prioritize capacity building can result in a dependency on external assistance, undermining local healthcare systems.
- Infrastructure Development
Investing in essential infrastructure supports sustainable healthcare delivery. Building or renovating clinics, providing access to clean water and sanitation, and establishing reliable supply chains contribute to a community’s long-term health and well-being. A program that constructs a well to provide clean drinking water for a rural village, in addition to providing medical services, addresses a fundamental health determinant and promotes lasting improvements. Conversely, simply providing medication without addressing underlying environmental factors offers only temporary relief.
- Community Engagement
Involving community members in the planning and implementation of medical initiatives ensures relevance and sustainability. Programs should actively solicit input from local leaders and residents to identify needs and tailor interventions accordingly. A community health program that relies solely on external expertise without engaging local stakeholders may face resistance and fail to achieve its goals. In contrast, a program that incorporates local knowledge and empowers community members to participate in health promotion activities is more likely to achieve lasting success.
- Economic Empowerment
Addressing economic disparities can significantly improve health outcomes and enhance the sustainability of medical initiatives. Programs that provide job training, microfinance opportunities, or support for local businesses contribute to economic stability and improve access to healthcare. A program that trains local women in sewing and provides them with sewing machines, in addition to providing medical care, empowers them to generate income and improve their families’ health and well-being. Neglecting economic factors can undermine the long-term effectiveness of medical interventions.
The interwoven nature of these elements reveals that a truly sustainable medical volunteer program focuses on comprehensive community development, not just episodic healthcare delivery. Initiatives must prioritize capacity building, infrastructure development, community engagement, and economic empowerment to achieve lasting positive change and avoid creating dependency on external resources.
5. Program Logistics
Program logistics constitute the operational framework underpinning the success of medical volunteer programs. These logistical elements directly influence the feasibility, efficiency, and ethical conduct of healthcare delivery in resource-limited settings. Inadequate planning and execution of logistical details can compromise patient safety, hinder program objectives, and damage the reputation of participating organizations. A comprehensive approach to program logistics encompasses a spectrum of considerations, including transportation, accommodation, supply chain management, communication infrastructure, and security protocols.
Real-world examples underscore the critical importance of robust program logistics. Consider a scenario where a medical team arrives at a remote clinic without adequate supplies of essential medications due to inadequate inventory management. The resulting inability to treat patients undermines the entire purpose of the program and may exacerbate existing health disparities. Conversely, a well-organized program that ensures a reliable supply of essential medicines, coupled with appropriate storage facilities and trained personnel to manage inventory, can significantly improve patient outcomes. Similarly, logistical challenges related to transportation, such as impassable roads or unreliable vehicles, can prevent medical teams from reaching patients in need, particularly in emergency situations. The establishment of secure transportation routes and contingency plans for logistical disruptions is therefore crucial for ensuring timely access to healthcare services.
In conclusion, program logistics are not merely administrative details, but rather fundamental determinants of the effectiveness and ethical integrity of medical volunteer programs. Careful planning, meticulous execution, and continuous monitoring of logistical elements are essential for maximizing positive impact and minimizing potential harm. Addressing logistical challenges proactively requires a collaborative approach involving program organizers, volunteers, local communities, and relevant stakeholders. This collaborative framework fosters a sustainable and ethically sound foundation for medical volunteer efforts, contributing to improved health outcomes and enhanced community well-being.
6. Financial Responsibility
Financial responsibility constitutes a cornerstone of ethical and effective medical volunteer programs. The financial aspects encompass a wide spectrum, from the program’s resource management to the participant’s personal financial considerations. Irresponsible financial practices can undermine program sustainability, compromise the quality of care delivered, and create ethical dilemmas. Programs require transparent budgeting, prudent allocation of resources, and adherence to strict accounting practices. Participants bear the responsibility of understanding the financial implications of their involvement, ensuring they do not incur undue personal debt or exploit program resources for personal gain.
Consider, for example, a program that lacks transparency in its financial dealings. Donations may be diverted for purposes unrelated to the program’s stated objectives, eroding donor trust and hindering the ability to attract future funding. Alternatively, a participant who misuses program resources, such as medications or supplies, for personal use violates ethical standards and compromises the program’s ability to serve the community effectively. Effective financial management includes the establishment of clear policies regarding the use of program funds, regular audits to ensure accountability, and training for volunteers on ethical financial conduct. Programs that prioritize financial responsibility are more likely to attract reputable donors, recruit qualified volunteers, and achieve sustainable positive impact within the communities they serve.
In summary, financial responsibility is not merely a practical consideration but an ethical imperative. Transparent financial practices, prudent resource management, and responsible conduct by all stakeholders are essential for maintaining program integrity, fostering donor trust, and ensuring the long-term sustainability of medical volunteer initiatives. Overlooking this critical component can jeopardize program effectiveness and undermine the very principles of humanitarian service.
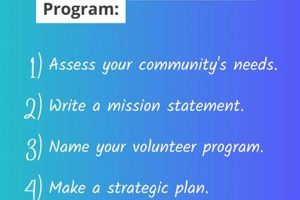
7. Community Needs
The nexus between community needs and medical volunteer programs represents a fundamental determinant of program efficacy and ethical justification. Community needs, encompassing the specific healthcare deficits and socio-economic factors impacting population health, serve as the primary impetus for the initiation and design of effective medical volunteer interventions. These needs, whether stemming from disease prevalence, inadequate access to essential services, or health disparities, dictate the scope, focus, and resource allocation of said programs. Programs operating without a thorough understanding and direct response to identified community needs risk ineffectiveness, irrelevance, and potential ethical breaches, expending resources without yielding meaningful or sustainable benefits. For example, a volunteer program offering specialized surgical procedures in a region where the primary health concern is malnutrition and infectious disease transmission reflects a disconnect between program activities and actual community requirements, diverting resources from more pressing needs.
Conversely, programs meticulously aligned with identified community needs demonstrate enhanced potential for positive and sustainable impact. Such programs prioritize comprehensive needs assessments, engaging local stakeholders to ascertain the most critical healthcare gaps and socio-economic determinants of health. A real-life instance includes a medical volunteer program addressing high rates of maternal mortality in a rural area. Through community consultations, the program identified key barriers to accessing prenatal care, including geographical isolation, lack of transportation, and cultural beliefs discouraging facility-based deliveries. Subsequently, the program established mobile clinics, trained local birth attendants, and conducted community education campaigns to address these specific barriers, leading to a measurable reduction in maternal mortality rates. This targeted approach, driven by community needs, underscores the practical significance of aligning program activities with the specific requirements of the population served.
In conclusion, a comprehensive understanding of community needs is not merely a preliminary step but rather an ongoing process integral to the design, implementation, and evaluation of medical volunteer initiatives. Failure to prioritize community needs can lead to misallocation of resources, ineffective interventions, and potential harm. Conversely, programs that meticulously align with community needs are better positioned to achieve sustainable positive impact, contributing to improved health outcomes and enhanced community well-being. The ongoing challenge lies in fostering authentic community engagement, ensuring that volunteer efforts are driven by the expressed needs and priorities of the population served, thereby maximizing the ethical and practical value of medical volunteer programs.
Frequently Asked Questions Regarding Medical Volunteer Programs
The following questions address common inquiries and concerns pertaining to organized medical service. The intent is to provide clear and objective information to facilitate informed decision-making.
Question 1: What constitutes a reputable medical volunteer program?
Reputable programs demonstrate transparent organizational structures, ethical operational guidelines, and a documented history of positive community impact. Accreditation by relevant regulatory bodies and endorsements from established healthcare organizations serve as indicators of program legitimacy.
Question 2: What are the primary ethical considerations in medical volunteer work?
Ethical conduct necessitates adherence to principles of beneficence, non-maleficence, respect for autonomy, and justice. Programs must prioritize patient safety, obtain informed consent, respect cultural sensitivities, and avoid exploiting vulnerable populations.
Question 3: What skills are most valuable for participants in medical volunteer programs?
Beyond medical expertise, valuable skills include adaptability, cultural sensitivity, communication proficiency, and problem-solving capabilities. Participants must be prepared to work in resource-limited settings and collaborate effectively with diverse teams.
Question 4: How can the sustainability of medical volunteer programs be ensured?
Sustainability depends on capacity building within local communities, infrastructure development, community engagement, and economic empowerment. Programs should prioritize long-term impact over short-term relief efforts, empowering local healthcare providers and promoting community ownership.
Question 5: What are the financial responsibilities associated with medical volunteer programs?
Participants may incur expenses related to travel, accommodation, insurance, and program fees. Programs must maintain transparent financial practices, demonstrating responsible resource allocation and adherence to ethical accounting standards.
Question 6: How can community needs be effectively addressed by medical volunteer programs?
Programs must conduct thorough needs assessments, engaging local stakeholders to identify the most pressing healthcare gaps and socio-economic determinants of health. Interventions should be tailored to specific community needs, promoting equitable access to healthcare services.
These FAQs provide a concise overview of key considerations for participation in organized medical service. Thorough research and careful planning are essential for ensuring a productive and ethical experience.
The following section will delve into case studies showcasing successful implementation and notable challenges within the realm of medical volunteer programs.
Conclusion
The preceding analysis has explored various facets of medical volunteer programs, emphasizing ethical considerations, skill application, cultural sensitivity, sustainability impact, program logistics, financial responsibility, and the critical importance of addressing community needs. These elements, when effectively integrated, constitute the foundation for impactful and responsible initiatives aimed at improving healthcare access and outcomes in underserved populations. Understanding these intertwined factors is paramount for both participating volunteers and the organizations that facilitate these endeavors.
The continued success and ethical standing of medical volunteer programs depend on a sustained commitment to responsible planning, transparent operations, and a dedication to empowering local communities. Future efforts should prioritize collaboration, knowledge sharing, and the rigorous evaluation of program outcomes to ensure that these initiatives continue to serve as a force for positive change in global health. The pursuit of equitable healthcare access demands a steadfast dedication to ethical principles and a genuine commitment to community-driven solutions.